
 current location: Index >> News >> company news >> Perioperative Ultrasound Training Guide (2020 Edition) Sharing and Preview of the Eighth National Training Course on Perioperative Ultrasound in West China Hospital
current location: Index >> News >> company news >> Perioperative Ultrasound Training Guide (2020 Edition) Sharing and Preview of the Eighth National Training Course on Perioperative Ultrasound in West China Hospital
 TEL:400-809-7996
TEL:400-809-7996
 Contacts:Mr. Jane
Contacts:Mr. Jane
Date:2020-10-28 Author:
Background and current situation
Ultrasound technology is increasingly widely used in the field of anesthesiology due to its advantages of simplicity, speed, practicality and repeatability. Ultrasound-guided nerve block and vascular puncture techniques, point-of-care ultrasound (POCUS) and perioperative echocardiography have all become indispensable clinical techniques in anesthesia.
In order to further regulate the scope of intraoperative ultrasound training and promote the safe, widespread and reasonable use of ultrasound technology in the perioperative period, the Ultrasonics Group of the Chinese Medical Association Anesthesiology Branch organized the preparation of a perioperative ultrasound training guide (2020 edition) for colleagues in anesthesia reference. Next, let's interpret the latest version of the perioperative ultrasound training guide (2020 version).

01
Ultra-sound guided neurological block and
Blood tube puncture technique
1. Trainees
(1) Have a physician qualification certificate and a physician practice certificate;
(2) Complete standardized training for residents.
2, training objectives
3. Training content and requirements
Using theoretical teaching, simulation teaching, clinical operation and practice, case discussion, etc., fill in the training records. The training time is 3 months.
4. Basic requirements
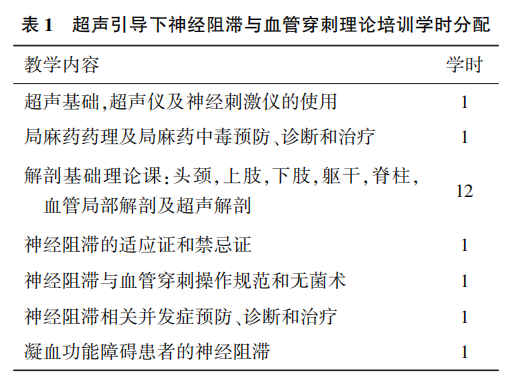
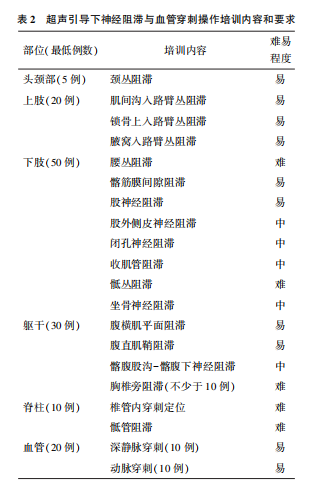
It is recommended that theoretical teaching is 18 class hours, simulated puncture training is 2 class hours, case-oriented clinical thinking training is 6 class hours, literature study is 6 class hours, each class is 45 minutes. Theoretical teaching includes the principles of ultrasound, pharmacology of local anesthetics, anatomical basis, and operation specifications of nerve block and vascular puncture (Table 1) [2-3]. The operation teaching content includes the block and puncture methods of upper limbs, lower limbs, trunk, spine and blood vessels. The learning process is arranged according to the principle of easy to difficult (Table 2) [4-5]
5. Higher requirements
1.3.2.1 Elective nerve block technique
includes the head and neck, upper limbs, lower limbs and trunk parts that are less used or difficult to operate (Table 3) [5]. Teaching is conducted according to the specific conditions of the training base and trainees, and there is no minimum number of cases.

6. Research and teaching ability training
(1) Encourage one clinical case report or review to be written within the training period of 3 months, complete one literature interpretation or one complete case discussion.
(2) Assist the teaching teacher to complete the teaching work for beginners. Participating in teaching activities should include theory teaching assistant, ultrasound simulation operation assistant, ultrasound clinical operation assistant and case discussion assistant.
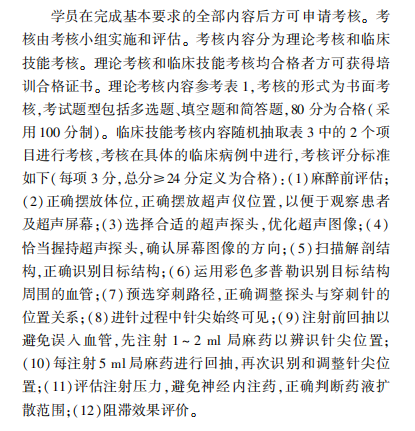
7, assessment method
02
Ultra sound beside the bed
1. Trainees
(1) Have a physician qualification certificate and a physician practice certificate;
(2) Complete standardized training for residents.
2, training objectives
Through the POCUS training that combines theory and practice, students can understand the basic principles of ultrasound imaging, correctly use ultrasound equipment and image optimization methods, can master the relevant theoretical knowledge of perioperative POCUS and correct clinical work methods, and master the importance of POCUS to important organs. evaluation of. On this basis, through the identification and evaluation of ultrasound images, individualized diagnosis and treatment plans can be formulated for perioperative patients [7]. During the training, good team communication skills should be obtained. At the end of the training, be able to independently engage in perioperative POCUS operation and evaluation.
3. Training content and requirements
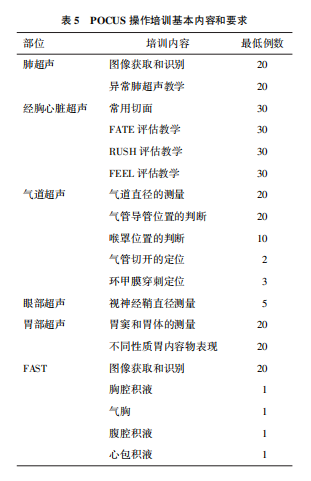
Training is carried out in the form of theory teaching, simulation teaching, clinical operation and practice, case discussion, etc., and the training records are filled in. The training time is 3 months. POCUS training should include six parts: lung ultrasound, transthoracic cardiac ultrasound, airway ultrasound, eye ultrasound, gastric ultrasound and focus assessed with sonography in trauma (FAST). Transthoracic cardiac ultrasound includes target-oriented ultrasound. Thoracic heart ultrasound (focus assessed transthoracic echocardiography, FATE), rapid ultrasound in shock (RUSH) for shock patients, and focus echocardiographic evaluation in life support (FEEL) [8-9]. It is recommended that each part of the training rotate for 1 to 2 weeks, and the training time and sequence should be adjusted according to the specific situation, but there should be no missing items.
4. Basic requirements
(1) POCUS theoretical study adopts the teaching method. The content of the teaching includes the evaluation methods, evaluation procedures, image interpretation, indications and case analysis of lung ultrasound, transthoracic heart ultrasound, airway ultrasound, eye ultrasound, gastric ultrasound and trauma ultrasound. During the three-month training period, theory courses must be completed. See Table 4 for specific class hours, 45 minutes per class hour.
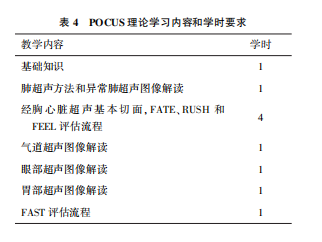
(2) See Table 5 for the basic requirements of POCUS clinical operation training. If the clinical case implementation training cannot be completed during the training, simulation training can be used instead.
5. Higher requirements
The training of the ability to handle complex clinical cases. Through learning, you can be more proficient in the rapid assessment of important organs, and through the interpretation of ultrasound image results, the damage to the airway and respiratory function, common heart diseases, hemodynamic disorders, Critical and difficult cases of abdominal trauma, intracranial hypertension, and stomach fullness should be appropriately treated clinically, and individualized perioperative patient diagnosis and treatment plans should be developed [10].
6. Research and teaching ability
Encourage writing a clinical case report within 3 months of training. Assist the teaching teacher to complete the teaching work for beginners. The teaching activities include case discussion assistant teaching, theory teaching assistant teaching, ultrasound clinical operation assistant teaching and ultrasound simulation operation assistant teaching.
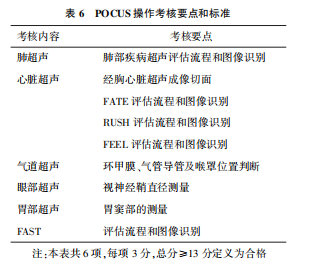
7, assessment method
After the basic training is over, you can apply for the completion assessment. The trainees submit the POCUS inspection register required to be completed during the training, and the clinical skills assessment can only be carried out after the assessment team has passed the assessment. The assessment includes two parts: professional theory and clinical skills assessment. The theoretical assessment content refers to the teaching content of Table 5, including POCUS basic knowledge, process and recognition of common ultrasound images. The test questions include multiple choice questions, fill-in-the-blank questions and short-answer questions, 80 points Qualified (using a 100-point system). The content of the operation assessment is to perform the six-part bedside ultrasound operation process in a specific clinical case. The content includes acquiring and optimizing POCUS images, assessing the condition of the disease, and making clinical decisions. Refer to Table 6 for the scoring criteria for operation assessment.
03
perioperative ultrasound cardiogram
1. Trainees
(1) Have obtained a physician qualification certificate and a physician practice certificate;
(2) Complete standardized training for residents;
(3) Have a solid knowledge of cardiovascular anatomy and pathophysiology, and understand the relevant surgical procedures.
2, training objectives
Through 3 months of training and learning, master the basic theory, basic knowledge and basic skills of perioperative echocardiography, and be able to independently perform complete and comprehensive echocardiography. Master the diagnosis and evaluation of common cardiovascular structural and functional abnormalities in patients undergoing non-cardiac surgery, and master the perioperative echocardiographic monitoring of cardiovascular surgery. Understand the echocardiographic evaluation of complex cardiovascular problems, and have the ability to provide perioperative cardiovascular ultrasound diagnosis, optimize perioperative management and diagnosis and treatment decision-making [11-12].
3. Training content and requirements
Use theory teaching, simulation teaching, clinical operation and practice, case discussion and other forms to fill in training records. The training time is 3 months.
4. Basic requirements
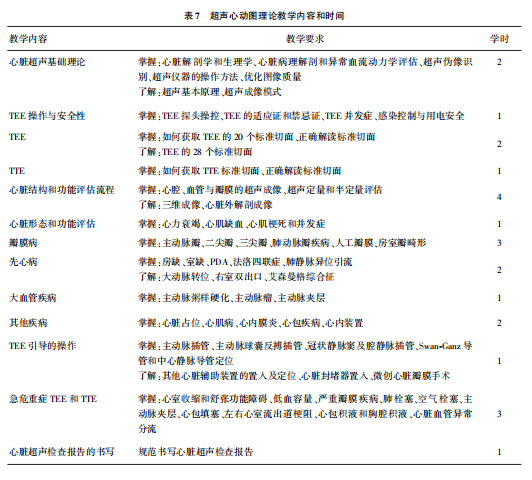
includes theoretical teaching and clinical operation, including 24 hours of theoretical teaching, 2 hours of simulation teaching, and 6 hours of interpretation of echocardiographic reports. 45 minutes per class hour.
Theoretical teaching can be divided into three stages
The first stage
The first stage introduces the normal heart ultrasound anatomy and physiology, basic ultrasound knowledge, transesophageal echocardiography (TEE), transthoracic echocardiography (TTE) basic section and spatial positioning, and left and right heart function evaluation.
second stage
The second stage introduces the evaluation of heart valve function, including mitral valve, tricuspid valve, aortic valve regurgitation and stenosis, paravalvular leak, anterior mitral valve systolic anterior motion (systolic anterior motion, SAM) signs and congenital Valve malformations; segmental ventricular wall motion abnormalities, ischemic valve regurgitation, ventricular aneurysms; atrial defect, ventricular defect, patent ductus arteriosus (PDA); pulmonary hypertension with right heart dysfunction, etc.
The third stage
The third stage introduces the application of heart valve surgery, ultrasound-guided atrioventricular occlusion, tetralogy of Fallot, double outlet of the right ventricle and other diseases, as well as large blood vessels, pericardial diseases, cardiomyopathy, heart occupying, etc.[13-15] (Table 7).
Clinical operation skills training needs to be completed on a large number of clinical cases, including the following
The esophageal ultrasound probe can be placed smoothly and safely;
A comprehensive esophageal ultrasound examination can be performed to obtain all 20 TEE standard sections;
can distinguish between normal heart structure and obvious abnormal structure ultrasound changes;
can correctly identify common ultrasound artifacts;
can identify and deal with common complications of transesophageal ultrasound; can distinguish left and right ventricular systolic and diastolic dysfunction;
can distinguish obvious segmental wall dyskinesia;
can distinguish the ultrasonic changes of air embolism and pulmonary embolism;
can evaluate changes in valve structure and function, and correctly evaluate the function of artificial valves;
Able to recognize the ultrasound manifestations of heart occupying;
can correctly identify pericardial effusion and pleural effusion;
can identify the ultrasound changes of ventricular volume status;
can identify the ultrasound changes of common congenital heart disease;
can guide the cardiac surgeon to perform coronary sinus catheterization, vena cava and aortic catheterization, intra-aortic balloon pump (IABP) and other ventricular assist devices placement and positioning;
can accurately communicate the patient's ultrasound changes with the surgeon;
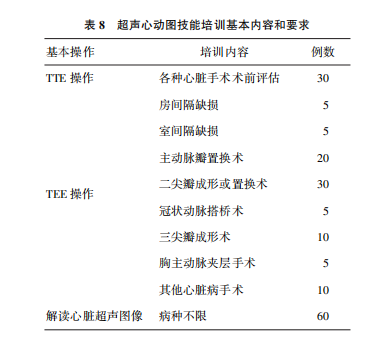
can perform cardiac ultrasound examinations of critically ill patients to identify critically ill patients such as severe ventricular dysfunction, hypovolemia, severe valve disease, outflow tract obstruction [16-19] (Table 8).
5. Higher requirements
(1) Clinical application-oriented skills training
On the basis of mastering the basic theory and operational skills of echocardiography, practical application-oriented clinical skills should be trained, such as hemodynamic ultrasound monitoring; TEE in minimally invasive valve surgery; TEE in hypertrophic obstructive Intraoperative application of cardiomyopathy; TEE diagnosis and decision-making in congenital heart disease surgery; TEE application in congenital heart disease closure surgery; TEE's guiding role in the process of detaching from cardiopulmonary bypass, etc. [20-22].
(2) Research and teaching ability training
Encourage to write at least one clinical case report within 3 months of training; assist the superior instructor to complete the teaching work for beginners. Teaching activities include case discussion assistant, theory class assistant, ultrasound clinical operation assistant and ultrasound simulation operation assistant.
6. Assessment method
After completing the 3-month clinical training, the trainees should submit the cardiac ultrasound case register and the cardiac ultrasound report required to be completed during the training, and the assessment can only be carried out after being qualified by the assessment team. The assessment includes two parts: theory and clinical skill assessment.
The theoretical assessment content refers to the teaching content in Table 8. The test questions include multiple choice questions, fill-in-the-blank questions and short-answer questions. 80 points are qualified (100 points system is used).
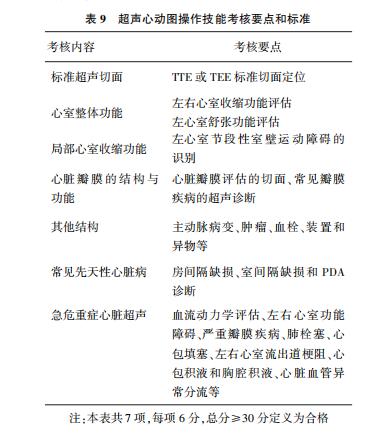
Clinical skills assessment is carried out in specific clinical cases, including the acquisition of standard ultrasound slices and image optimization of cardiac ultrasound, the identification of ultrasound slices related to the pathophysiological changes of the disease, the application of TEE in common cardio-macrovascular surgery, and hemodynamic monitoring The clinical operation skills required to master such as evaluation and evaluation (Table 9).
List of experts in perioperative ultrasound training guidelines:
principal
Wang Ji (Department of Anesthesiology, Xiangya Hospital, Central South University)
Zhu Tao (Department of Anesthesiology, West China Hospital, Sichuan University)
Jin Liu (Department of Anesthesiology, West China Hospital, Sichuan University)
Writer
Wanli (Department of Anesthesiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology)
Yu Hui (Department of Anesthesiology, Beijing Hospital)
Bian Jinjun (Department of Anesthesiology, Changhai Hospital, Naval Military Medical University)
Wang Ruike (Department of Anesthesiology, Xiangya Hospital, Central South University)
Expert group members (arranged in alphabetical order of surnames)
Cui Xulei (Department of Anesthesiology, Peking Union Medical College Hospital)
Duan Xuefei (Department of Anesthesiology, Guangdong Provincial People's Hospital)
Feng Xia (Department of Anesthesiology, The First Affiliated Hospital of Sun Yat-sen University)
Fu Qiang (Department of Anesthesiology, General Hospital of PLA)
Gong Maowei (Department of Anesthesiology, General Hospital of PLA)
Ji Fuhai (Department of Anesthesiology, The First Affiliated Hospital of Soochow University)
Li Ping (Department of Anesthesiology, West China Hospital, Sichuan University)
Li Yingyuan (Department of Anesthesiology, The First Affiliated Hospital of Sun Yat-sen University)
Liu Huayue (Department of Anesthesiology, The First Affiliated Hospital of Soochow University)
Shangyou (Department of Anesthesiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology)
Song Haibo (Department of Anesthesiology, West China Hospital, Sichuan University)
Tang Shuai (Department of Anesthesiology, Peking Union Medical College Hospital)
Wang Aizhong (Department of Anesthesiology, Shanghai Sixth Hospital)
Wang Sheng (Department of Anesthesiology, Guangdong Provincial People's Hospital)
Zhu Maoen (Department of Anesthesiology, Xiangya Hospital, Central South University)
The eighth national training course on perioperative ultrasound of the Ultrasound Group of the Anesthesiology Branch of the Chinese Medical Association begins~?
01 Teaching time: 2020.11.04-06
With the rapid development of perioperative medicine, anesthesia disciplines around the world have introduced ultrasound imaging technology. To promote the application of ultrasound visualization technology in perioperative medicine, it is sponsored by the Ultrasound Group of the Chinese Medical Association Anesthesiology Branch, Shenzhen Camel Biomedical The Eighth National Perioperative Ultrasound Training Course of the Ultrasound Group of the Chinese Medical Association Anesthesiology Branch, co-organized by the electronics company, will be held at West China Hospital from November 4 to 6, 2020.
02 Suitable object
Anesthesia and pain scientists, critical/emergency doctors, cardiologists/surgeons, etc. who plan to develop ultrasound business.
03 Notice for registration
Registration method: Individual registration or collective registration by hospital
Number of trainees: 16 students or more, the maximum limit is 24
-END-




 400-809-7996
400-809-7996  tuoren@tuoren.com
tuoren@tuoren.com
Address: 405, building 1, Biomedical Innovation Industrial Park, No. 14, Jinhui Road, Pingshan District, Shenzhen